The Burning Issue 1
UV and Skin CancerUV and Skin Cancer
“Surfers, swimmers and paddle boarders are six times more likely to develop melanoma than the general population, according to a study by the Southern Cross University in Australia.”
The importance of sun protection should not be underestimated. Skin cancer is the most preventable cancer, with over 95% of skin cancers, including melanoma, the most deadly form of skin cancer, being caused by the sun’s ultraviolet (UV) rays.[1]
Sadly, however, skin cancers, including melanoma, are the most common cancer in people. In 2020, an estimated 325,000 new cases of melanoma were diagnosed worldwide and 57,000 people died from the disease. These figures are quite horrendous when one considers that while no cancer is 100% preventable, the incidence of melanoma could be significantly reduced through people taking proactive, preventative measures such as protecting their skin from sun emitted UV rays and avoiding artificial UV sources such as tanning beds and sunlamps.
Some telling global melanoma facts:
- 1 Australian is diagnosed with melanoma every thirty minutes and another dying from it every six hours. Melanoma is particularly ubiquitous as it affects people of all ages and is the most common cancer diagnosed in Australians aged 20 to 39.
- Skin cancer is the most common cancer affecting New Zealanders (population 5.2 million) with 80,000 people being diagnosed each year, accounting for 80 percent of all new cancers. Melanoma is the third most common cancer in men and women in New Zealand. 6,000 melanomas are diagnosed in New Zealand every year
- Skin cancer is the most common cancer in the United States. One in five Americans will develop skin cancer in their lifetime. Approximately 9,500 people in the U.S. are diagnosed with skin cancer every day. This means that about 3.5 million Americans are diagnosed with skin cancer each year. It is estimated that 7,990 deaths (5,420 men and 2,570 women) from melanoma will occur in the United States in 2023
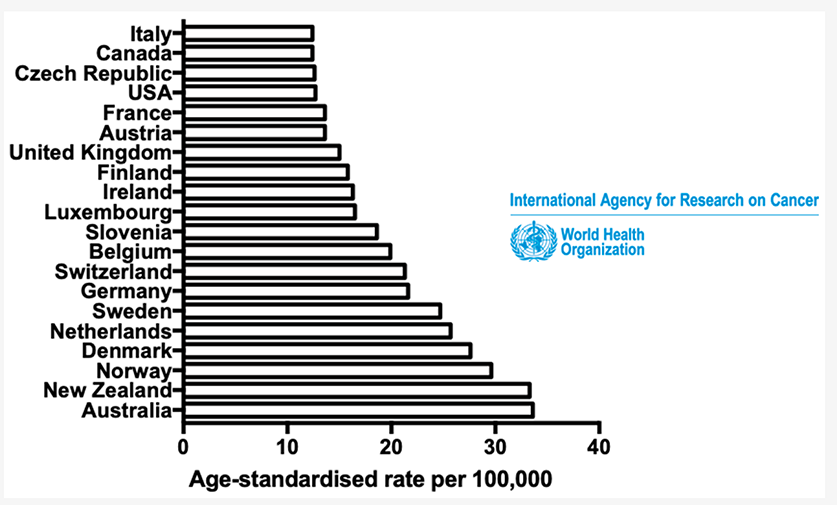
- People tend to think that only regions with long, hot summers have high rates of UV related skin cancer. However, from a global perspective, while the highest rates of melanoma occur in Australia, closely followed by New Zealand, Denmark comes in third, the Netherlands fourth with Norway fifth
MELANOMA RISK FACTORS
Most at risk of developing melanoma
- An Australian study found surfers, swimmers and paddle boarders are six times more likely to develop melanoma than the general population
- Other studies have shown that outdoor workers are 2.5 – 3.5 times more likely to develop skin cancer than indoor workers. In 2023, the WHO and the International Labour Organization jointly announced that nearly 1 in 3 deaths from non-melanoma skin cancer are caused by UV radiation from outdoor work. Non-melanoma skin cancer refers to a group of cancers that develop in the upper layers of the skin, beyond the melanocyte cells that produce pigment.
- Fair skinned people are at higher risk when compared to darker complexions. However, a recent review of skin cancer in patients with darkly pigmented skin showed that mortality rates in this population are substantially higher than in those with lighter skin, as a result of delayed presentation, and that 60% of respondents with darkly pigmented skin believed that they were not at risk of skin cancer
- High UV exposure significantly increases risk
- People with childhood high levels of ultraviolet (UV) exposure and episodes of sunburn in childhood are at increased risk
- People who use solariums are at increased risk of developing melanoma
- Males are at higher risk than females. The American Academy of Dermatology notes by age 65, men are two times more likely as women of the same age to get melanoma. By age 80, men are three times more likely than women of the same age group to develop melanoma
- People who have a family history of melanoma are at increased risk
- Melanoma is more common in older people due to cumulative UV exposure, with every decade of sun exposure shown to further increase risk
UV Exposure
Exposure to ultraviolet (UV) rays is a major risk factor for most melanomas. For example, in Australia, up to 95% of melanomas are attributable to overexposure to UV radiation.
Sunlight is the main source of UV rays. Tanning beds and sun lamps are also sources of UV rays. While UV rays make up only a very small portion of the sun’s rays, they are the main cause of the damaging effects of the sun on the skin.
People who live at high altitudes or in areas with bright sunlight year-round have a higher risk of developing skin cancer. People who spend a lot of time outside also have a higher risk. For example, surfers, swimmers and paddle boarders are six times more likely to develop melanoma than the general population, according to a study by the Southern Cross University in Australia, while other studies have found that outdoor workers are 2.5 – 3.5 times more likely to develop skin cancer than indoor workers.
People with childhood high levels of ultraviolet (UV) exposure and episodes of sunburn in childhood also are at increased risk.
Fair skinned people
People with fair skin are at higher risk of developing skin cancer than people with darker complexions . This risk is also higher for people whose skin has a tendency to burn rather than tan.
UV radiation does affect dark skin and can cause DNA damage; however, the damage is seven to eight times lower than the damage done to white skin, given the natural sun-protective effect of increased melanin in darker skin. However, as previously noted, a recent review of skin cancer in patients with darkly pigmented skin showed that mortality rates in this population are substantially higher than in those with lighter skin, as a result of delayed presentation, and that 60% of respondents with darkly pigmented skin believed that they were not at risk of skin cancer.
Sunburn
While sunburn does not directly cause melanoma, it is often used as an indicator of melanoma risk. This is because it is memorable and is a marker of the type of sun exposure most associated with melanoma (intermittent intense exposure) combined with the type of skin that is most susceptible to melanoma (skin that is sensitive enough to UV to burn). A study by Pfahlberg and Kölmel found that having more than five sunburns doubled the risk of melanoma, with risk similar for childhood exposure before 15 years of age, and exposure after 15 years of age.
Solarium Use
A systematic review has shown a dose-response relationship between sunbed use and melanoma risk. Sunbed use increases melanoma risk by 20%, with an increase of 59% if used before 35 years of age. A study in the USA found that the more frequently people used solariums, the higher their risk of melanoma – regardless of the age at which they began using solariums.
Family history
About 10% of people with melanoma have a family history of the disease.
Age
Melanoma is more common in older adults than younger people, with the mean diagnosis age being 66 years among men and 62.3 years among women in 2018.
Older adults have had more cumulative sun exposure than younger people, with every additional decade of high sun exposure shown to further increase the risk of melanoma.
Global UV Levels
The highest levels of UV occur in equatorial regions. Closer to the equator the sun’s rays have a shorter distance to travel through the atmosphere and therefore less of the harmful UV radiation (UVR) can be absorbed.
Second to equatorial regions, southern hemisphere regions receive the highest UV at about 15% more UV radiation than the equivalent northern latitude regions.
Notably, the highest levels of melanoma occur in Australia (number 1) and New Zealand (close 2nd). Both countries being in the Southern Hemisphere while the Northern parts of Australia are equatorial, with Queensland being the skin cancer capital of Australia. We’ll talk more about global incidence of melanoma shortly. For now, see the following data that lists prevalence of melanoma per country.
Population Attributable Fraction (PAF) of melanoma cases worldwide in 2018, among men and women, attributable to UV radiation exposure, by country.
Stratospheric Ozone and UV
UV levels have significantly increased over the last 30 years due to depletion of the stratospheric ozone layer and global climate change. When ozone levels are depleted, the atmosphere loses its protective filter resulting in more solar UV radiation – particularly UVB – reaching the Earth’s surface. It has been calculated that for each 1% reduction in ozone there is an increase in UV radiation of about 1.2%.
As a result of ozone depletion, in the tropics, UV increase has been minimal, but in the mid-latitudes it has been more obvious. During the summer, for example, UV has increased by more than 20 percent in Patagonia and the southern portions of South America. It has risen by nearly 10 percent in Buenos Aires. At Washington, D.C.’s latitude — about 35 degrees north — UV has increased by about 9 percent since 1979. In Australia there has been an overall annual increase in UV levels of 2% to 6% since the 1990s, for locations throughout Australia.
Altitude and UV
With increasing altitude less atmosphere is available to absorb UV radiation. With every 1000 m in altitude, UV levels increase by approximately 10 per cent.
Time of day
UV levels vary mainly with the height of the sun in the sky and in mid-latitudes are highest during the summer months during the 4-hour period around solar noon. During these times the sun’s rays take the most direct path to earth. In contrast, during early morning or late afternoon hours the sun’s rays pass at a greater angle through the atmosphere. Much more UV radiation is absorbed and less reaches the Earth.
While not always possible, minimising exposure to ultraviolet (UV) radiation from the sun is the most effective strategy to prevent skin cancer. This includes planning outdoor activities to occur outside of the peak UV period (2 hours either side of solar noon), when an estimated 60% of the day’s UV radiation occurs. Around midday, skin will burn more quickly, and be exposed to more UVA as well as UVB, than earlier or later in the day. Outside of these times, the UV can still be intense, so sun protection is necessary for all times when the UV index is 3 or above.
Clouds and Haze
UV levels are highest under cloudless skies, and cloud cover generally reduces a person’s exposure. However, light or thin clouds have little effect and may even enhance UV levels because of scattering. Don’t be fooled by an overcast day or a cool breeze! Even a long stay in open shade, for example between buildings, may give a sensitive person a sunburn on a day with high UV levels.
Ground Reflection
UV radiation is reflected or scattered to varying extents by different surfaces, e.g. snow can reflect as much as 80% of UV radiation, dry beach sand about 15%, and sea foam about 25%.
Don’t Confuse Heat with UV
While there is a general perception that UV feels hot, based on the energy level of the UV rays, they may in fact be considered as cold rays. The heat felt on the skin on a sunny day is mostly due to the infrared radiation, with a caveat that after prolonged exposure, the UV radiation may start to cause damage to the skin, and therefore the skin irritant effect may be indirectly attributed to the UV radiation.
It’s often the cooler days that result in the worst sunburns because the UV level is high while the temperature is not. It can be hard to mentally disconnect heat and UV because when it is hot our skin does feel like it is burning, but in reality, the heat we are feeling is the infrared radiation which does not cause sunburn. Damaging UV is invisible and cannot be felt.
See image below that demonstrates UV levels in different geographic locations. The yellow regions show potentially extreme levels of UV (during the summer months) with red (Peruvian Andes and throughout the Altiplano region in South America) being very extreme. All sites between about 50° S and 40° N experience extreme UV (>10) at some stage of the year.
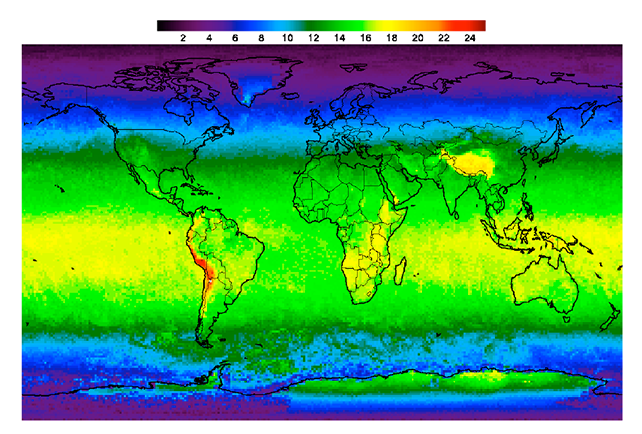
Image source: Liley, J. & McKenzie, Richard. (2006). Where on Earth has the highest UV?
Melanoma Prevalence Globally
Australia and New Zealand
New Zealand and Australia have the highest incidence of melanoma in the world, which is heightened by mostly fair skinned population and a climate that encourages outdoor lifestyles and sun-seeking [5]. High UV intensities also play a part in Australia with the equatorial regions of Australia recording the highest rates of melanoma.
In 2007 in New Zealand, from a total population of 4 million people, 2,173 people were registered with melanoma and 292 people died from the disease, whereas in Australia, a country of 21 million inhabitants (at that time), 10,342 people were diagnosed with melanoma and 1,279 died from it.
One Australian is diagnosed with melanoma every 30 minutes. More than two in three Australians will be diagnosed with skin cancer in their lifetime. In 2018, 15,344 new cases of melanoma were diagnosed in Australia, and in 2020, 1,401 people died as a result of melanoma.
The development of melanoma is more common as Australians grow older; however, it also develops in younger Australians, including those younger than 30 years old. Melanoma is the most common cancer in young Australians aged between 15 to 39, making up 20% of all of this group’s cancer cases.
Exposure to UV via sun exposure is estimated to cause around 95% of melanoma cases in Australia [6] and excessive childhood sun exposure may impart a particularly high risk for developing melanoma.[7]
North America
In 2019, there were an estimated 1,361,282 people living with melanoma of the skin in the United States. [8]
According to U.S. national cancer incidence data, invasive melanoma is among the 10 most common invasive cancers for both men and women.[9]
Skin cancer incidence has been increasing. The number of persons treated for all skin cancers combined increased by 44% from the period 2002–2006 to 2007–2011. The incidence of melanoma has been increasing for several decades, with rates doubling between 1982 and 2011. Mortality rates have remained relatively stable, although rates have risen slowly among males.[10]
The American Cancer Society’s estimates for melanoma in the United States for 2023 are:
- About 97,610 new melanomas will be diagnosed (about 58,120 in men and 39,490 in women).
- About 7,990 people are expected to die of melanoma (about 5,420 men and 2,570 women).
Melanoma is about 20 times more common in white than in black people in the United States. Overall, the lifetime risk of getting melanoma is about 2.6% (1 in 38) for Whites, 0.1% (1 in 1,000) for Blacks, and 0.6% (1 in 167) for Hispanic. However, while skin cancers are less prevalent in non-white racial ethnic groups, when they do occur, they tend to be diagnosed at a later stage and, as a result, have a worse prognosis. One study, for example, found an average five-year melanoma survival rate of only 67 percent in Black people versus 92 percent in white people.
Although melanoma does disproportionally affect Caucasian Americans, the incidence of disease can vary considerably depending on the geographic location of the population.[11]
UK and Europe
Melanoma claims annually more than 20,000 lives in Europe and is an important public health burden.[12] The incidence of melanoma skin cancer in people under the age of 55 years in Europe varies considerably among countries. The highest incidence is found in northern and western Europe and the lowest in southern European countries with rates from three to eight times lower for men and women respectively. In eastern European countries, incidence is low to intermediate (WHO). However, important differences in the sources and availability of accurate data exist among European countries and regions, contributing to a heterogeneous picture with 20-fold differences in the reported national melanoma incidence rates, divergent mortality trends, and solid disparities in survival across the continent.
Where the UK is concerned, according to the British Association of Dermatologists, the National Health Service (NHS) Digital data released as part of the National Disease Registration Service (NDRS) Get Data Out (GDO) programme shows that there were 224,000 skin cancers in England in 2019 and over 1.4 million skin cancers between 2013-2019. This makes skin cancer the most common cancer diagnosed in England.
The data shows that the incidence of skin cancer in England has increased from 177,677 in 2013 to 224,092 in 2019, a 26.1% increase over six years. While it is not possible to give a definitive explanation for this increase, it is likely that the ageing population, changing sun exposure behaviours and improvements to cancer registration may be responsible.
Asia
Melanoma incidence is lower in East and Southeast Asia as compared to North America or Europe with age-standardized rates of melanoma in the region averaged about 0.4–0.5/100 000 persons, as opposed to 8.6–13.8/100 000 persons for Europe and North America.[13] However, East and Southeast Asia is home to almost one-third of the global population, and therefore a significant burden of disease exists in terms of absolute patient numbers. Furthermore, the clinical evidence indicates that Asian melanoma patients typically present with more advanced disease, and their prognosis is generally worse than Caucasian patients.[14]
Lower rates of melanoma per head of population in Asia when compared to Europe and Nth America are a result of genetic factors along with lifestyle choices (e.g. many Asians avoid skin sun exposure).
References
[1] Prevent Cancer Foundation. Skin cancer. Available at: https://www.preventcancer.org/education/preventable-cancers/skin-cancer/
[2] Brenner M, Hearing VJ. The protective role of melanin against UV damage in human skin. Photochem Photobiol. 2008;84(3):539–49.
[3] Everett MA, Yeargers E, Sayre RM, Olson RL. Penetration of epidermis by ultraviolet rays. Photochem Photobiol. 1966;5(7):533–42
[4] Whiteman DC, Neale RE, Aitken J, Gordon L, Green AC, Janda M, Olsen CM, Soyer HP; Sunscreen Summit Policy Group. When to apply sunscreen: a consensus statement for Australia and New Zealand. Aust N Z J Public Health. 2019 Apr;43(2):171-175. doi: 10.1111/1753-6405.12873. Epub 2019 Jan 25. PMID: 30681231.
[5] Liley, J. & McKenzie, Richard. (2006). Where on Earth has the highest UV?
[6] Olsen CM, Wilson LF, Green AC, Bain CJ, Fritschi L, Neale RE, Whiteman DC. Cancers in Australia attributable to exposure to solar ultraviolet radiation and prevented by regular sunscreen use. Aust N Z J Public Health 2015; 39:471-6.
[7] Nikolau V, Stratigos AJ. Emerging trends in the epidemiology of melanoma. Br J Dermatol. 2014;170:11–19.
[8] National Cancer Institute. Cancer Stat Facts: Melanoma of the Skin found at https://seer.cancer.gov/statfacts/html/melan.html
[9] US Cancer Statistics Working Group. [Accessed July 4, 2016];United States cancer statistics: 1999–2012 incidence and mortality Web-based report.
[10] Watson M, Holman DM, Maguire-Eisen M. Ultraviolet Radiation Exposure and Its Impact on Skin Cancer Risk. Semin Oncol Nurs. 2016 Aug;32(3):241-54. doi: 10.1016/j.soncn.2016.05.005. Epub 2016 Jul 29. PMID: 27539279; PMCID: PMC5036351
[11] Matthews NH, Li WQ, Qureshi AA, et al. Epidemiology of Melanoma. In: Ward WH, Farma JM, editors. Cutaneous Melanoma: Etiology and Therapy [Internet]. Brisbane (AU): Codon Publications; 2017 Dec 21. Chapter 1.
[12] Forsea AM. Melanoma Epidemiology and Early Detection in Europe: Diversity and Disparities. Dermatol Pract Concept. 2020 Jun 29;10(3):e2020033. doi: 10.5826/dpc.1003a33. PMID: 32642304; PMCID: PMC7319793.
[13] Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, cancer incidence and mortality worldwide. Lyon, France: International Agency for Research on Cancer; 2013. Available from http://globocan.iarc.fr/Default.aspx. Accessed on July 21, 2016.
[14] Melanoma landscape in Asia-Pacific (2021). Novotech.